Rahul Sharma, MD, MBBS, FRACP
Assistant Professor of Medicine, Stanford University
Director of Structural Interventions, Stanford Health Care
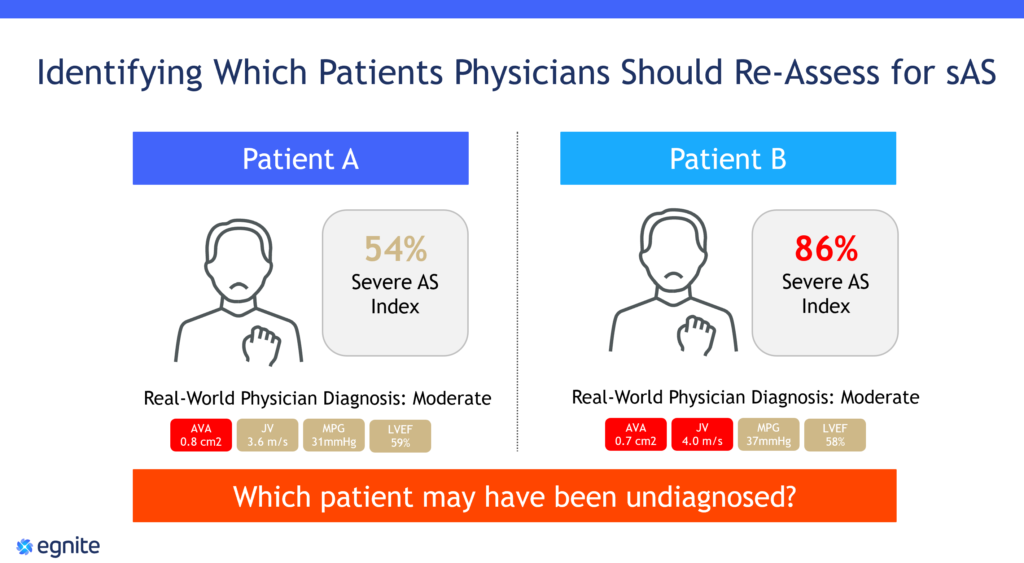
We’re all familiar in clinical practice with many patients who, at least on first glance, look the same. If you look at the output of the echo report and database, two patients appear to fall under the moderate AS category but may have been undiagnosed with severe AS. The CardioCare platform applies predictive algorithms to determine which patient has a higher chance of having undiagnosed severe AS, enabling physicians to quickly prioritize these patients for a second review.
CardioCare is not intended for use in diagnosis, cure, mitigation, treatment or prevention of structural heart disease. Product intended for secondary clinical review.
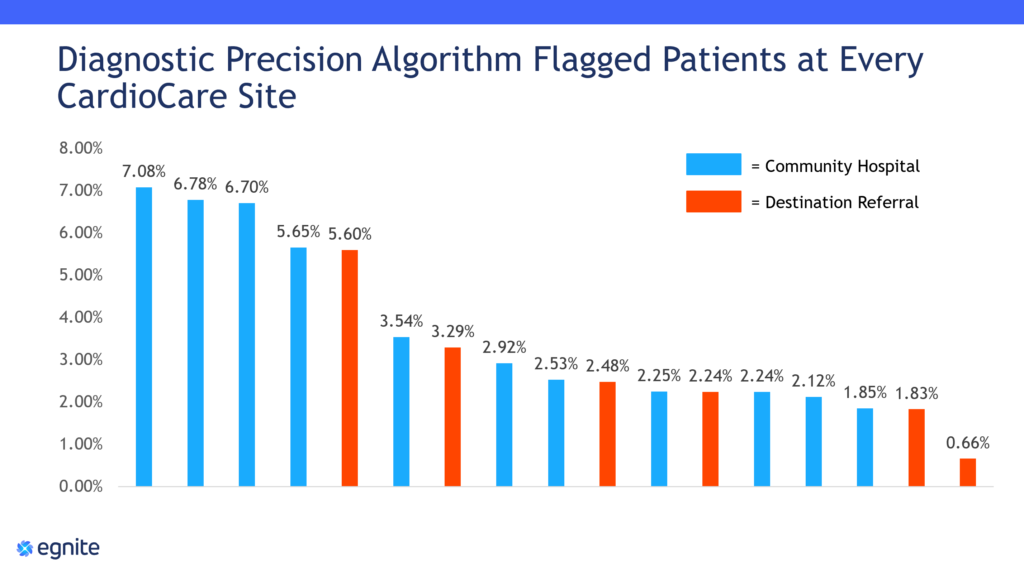
Early data from the CardioCare platform’s algorithm show significant variability in the percentage of patients flagged at each participating site. There is opportunity to reduce variability in diagnoses everywhere, regardless of big destination referral centers or rural community hospitals.
By identifying patients sooner, we can quickly place our patients on the appropriate care pathway, leading to better outcomes and a happier, healthier patient. With such large patient populations, it can be a challenge for structural heart programs to manage severe patients, while providing proactive surveillance for moderate patients that progress at different rates. The CardioCare platform has made it easy for our team to prioritize our large patient population and provide life saving therapies before these patients become too sick to treat.
Watch my presentation below to learn more.
#DigitalHealth #PrecisionMedicine #ArtificialIntelligenceSolutions