Soundos Moualla, MD, FACC, FSCAI
Interventional Cardiology
Dignity Health, Yavapai Regional Medical Center
Congestive heart failure (CHF) results in poor patient outcomes and increases the cost of care particularly with recurrent CHF hospitalizations. Using the CardioCare platform, we have started prospectively cross-matching the CardioCare alerts with hospital heart failure admissions for both aortic stenosis (AS) and mitral regurgitation (MR) patients. This has allowed us to provide better patient care by creating a daily alert system, that improved communication and coordination of care with the heart failure team at Dignity Health, Yavapai Regional Medical Center. This process led to more expeditious care of acutely ill patients, subsequently reducing re-admission rates of patients with congestive heart failure.
In the last year, 224 patients diagnosed with severe mitral regurgitation were also admitted to the hospital with heart failure. With this data, our team created a hybrid care plan among multiple clinical disciplines to increase disease awareness, implement therapeutic interventions based on guidelines, and improve the outcomes of this patient population.
Below is an example of sample data from the CardioCare platform, with reconciled plan of care:
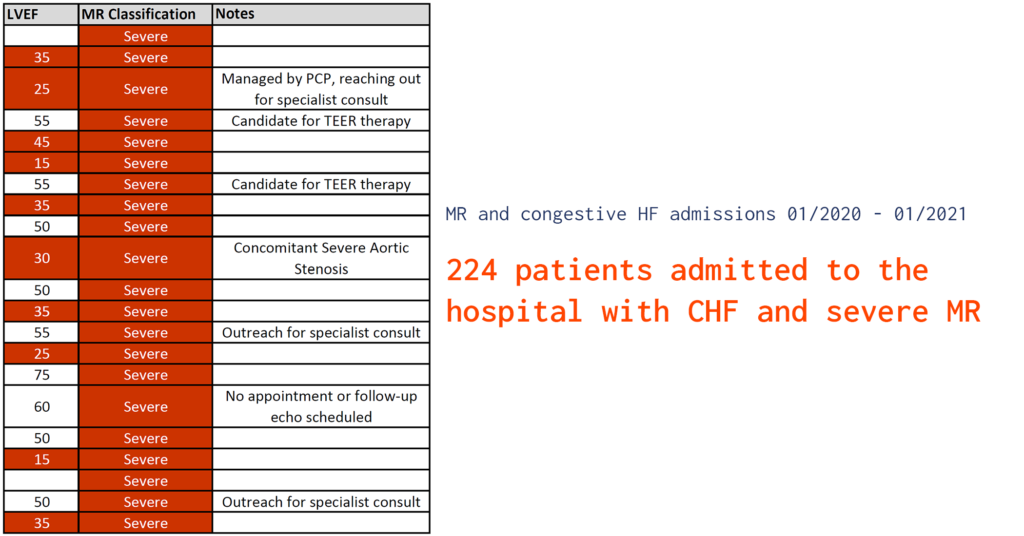
*Illustrative Data
In addition to the approach above, we plan to further collaborate with the heart failure team to look at patients with retrospective CHF admissions; specifically recurrent CHF admissions, and cross-match with aortic stenosis and mitral regurgitation patients from CardioCare. We anticipate that we will identify patients with untreated valve pathologies (AS and/or MR) with recurrent CHF exacerbations, who previously have not been under the care of the structural heart or heart failure teams. The aim is to ensure these patients are managed appropriately with guideline directed medical therapy, appropriate valvular therapies, and followed appropriately. It is critical for community structural heart programs to have a multifaceted approach to cardiovascular patient care, striving to improve the standards for physicians, allied health organizations, and most importantly patients.