Heart teams may see up to 25% more severe aortic stenosis patients
On the heels of the exciting EARLY TAVR data and egnite’s Acute Valve Syndrome in Aortic Stenosis study, both led by Dr. Philippe Genereux, we’ve been asked by several cardiovascular (CV) administrators what a potential change in the management of asymptomatic severe aortic stenosis (SAS) patients could mean for their already busy heart teams. Luckily, here at egnite, we have a lot of data. 34,000+ severe AS patient records’ worth of data. Combine that with 10+ years working with hospitals through our CardioCare® digital health platform, and we think we have a unique viewpoint of the market.Key Takeaways
In a landscape where recent trial data influences FDA approvals, updates to National Coverage Determinations (NCDs), AHA/ACC guidelines, and widespread adoption of this new evidence by the clinical community for the management of asymptomatic severe aortic stenosis (AS) patients:- Heart teams may experience a 19-25% increase in evaluation appointments.
- Implanters could perform 5-17% more aortic valve replacement (AVR) procedures, with 60-80% of these cases going to transcatheter aortic valve replacement (TAVR).
The Final Breakthrough of the Sizeable ‘Not Symptomatic Enough’ SAS Patient Cohort
We predict that the largest influx of patients will come from the cohort currently living with Class I indicated symptomatic aortic stenosis (AS), who are often classified by their cardiologists as ‘asymptomatic’ or ‘not symptomatic enough’ to justify intervention. This determination is frequently made without the use of a stress test and despite symptoms like fatigue, dizziness, and syncope that could suggest worsening disease. Symptom status is commonly logged in written physician notes. This assessment creates a key barrier to hospitals performing any further outreach to the MD or patient to coordinate a specialist evaluation for the patient’s progressive and sometimes deadly severe aortic stenosis. In our experience, there are two main headwinds for this patient cohort: very conservative (‘Partner 1’) cardiologists and the variability in how symptoms can drive actions with the average cardiologist. On a positive note, there may be an additional tailwind for this cohort with the complimentary egnite data published at TCT outlining improved outcomes for earlier treatment with AVR which we hope can support accelerated practice change.Headwind #1: ‘Partner 1’ Conservative Cardiologists
Our experience on the ground operationalizing the CardioCare platform and working with clinicians has made it clear that symptom status for AS has been a clinical grey area. Many programs we work with demonstrate a higher threshold than others in determining whether a patient is ‘symptomatic enough’ to warrant a heart team consult and even treatment. This can be especially pronounced for programs with a very conservative cardiology base, which is more common than one might think. We were recently in discussions with a health system that benchmarked in our bottom quartile for SAS treatment nationally, where 1 in 4 untreated SAS patients were deemed ‘asymptomatic’ by the managing physician. Our investigation revealed that most of these patients had 2 or more aortic stenosis symptoms recently logged in the electronic medical record and no stress test or thorough clinical interrogation of lifestyle adaptations. If this site practiced more like a top quartile site, 25% more patients would receive treatment in the coming year for their SAS. The program acknowledged their cardiology providers are more conservative in practice, and that some were still practicing with a ‘Partner 1 mentality’i. We can attest that many programs are faced with this therapy development challenge.Headwind #2: Symptoms Inspire Action Inconsistently… It Often Depends on the Symptom!
At egnite, we can also quantify that not all severe AS symptoms inspire action in the same way, even though permanent cardiac damage is often underway and getting worseii. Diagnosed severe AS patients presenting with angina (5% of patients) are +29% more likely to be treated at 180 days than a patient presenting with syncope (11% of patients) even though both these symptoms are classified in the guidelines as warranting at least a heart team consult if not treatmentiii. We’ve seen countless times patients with ICD.10 codes of the ‘softer’ symptoms – syncope, fatigue, dizziness – being labeled in the notes by their managing provider as ‘asymptomatic’ without a stress test or detailed interrogation of the patient’s lifestyle adaptations.Tailwind #1: Massive Database Provides Convincing Evidence that Earlier Treatment of SAS Improves Patient Survival by 3x
The Acute Valve Syndrome in Aortic Stenosis study presented at TCT demonstrates that progressive valve syndrome (PVS) or acute valve syndrome (AVS) at the time of AVR were associated with increased mortality or recurrent hospitalization with heart failure 2-years after AVR, compared to patients undergoing AVR while asymptomatic. Notably, asymptomatic SAS patients treated with AVR had a 3x increase in survival at two years vs. patients who already had symptoms before their AVR. The combination of the EARLY TAVR trial data and this study of over 17,000 AVR recipients makes a strong case for timely specialist evaluation and consideration of treatment for all severe AS patients, regardless of how conservative the cardiologist is, or which symptom is presenting. The authors hope dissemination of this evidence will make the following mentality clear: don’t wait for symptoms before sending SAS patients to the heart team.Our Estimates
Nationally, our data show that 80% of SAS patients are symptomatic, and over a 365-day period, 58% are treatediv. This leaves 22% who are untreated with documented symptoms. Predicting heart team referral rates from conservative cardiologists resulting from new data over the near term is a difficult task. Heart programs, the AHA/ACC associations, and medical device manufacturers will have their work cut out for them to support therapy awareness efforts. If we assume that the message gets out to 50-66% of these patients and their providers that regardless of the presence of symptoms, they should be seen by a heart team, then we could expect 11-15% more heart team encounters for severe AS. Heart team treatment rates nationally vary by how progressive the heart team is; we see a range of 25%-68% nationally, translating to an additional 3-10% in AVR volume. We’d argue this segment would err more heavily toward TAVR, if we assume some of the reluctance to refer can be attributed to patient frailty and attribution of symptoms to other high-risk comorbidities.The Smaller Opportunity – On-Paper ‘Asymptomatic’ SAS Patients
Our Estimates
This is the smaller segment since a truly asymptomatic SAS patient is so uncommon. We see that 20% of current ‘treatable’v SAS patients have 0 or 1 symptomsvi coded in the EMR and about 47% are treatedvii, 66% with TAVR proceduresviii: this group is our proxy for on-paper ‘asymptomatic’ patientsix. This nets us a potential group of 11% of patients in the population who may come into clinic. Of course, not every patient will choose to be evaluated if they aren’t experiencing symptoms. Given our symptomatic evaluation rate nationally is about 80%, let’s assume 50-66% of these asymptomatic patients are activated over the coming years and make their way into the heart team. This would result in a 5-7% increase in heart team consults and a 1-5% increase in treated patients, depending on the program.What About Moderate-to-Severe Aortic Stenosis?
Our Estimates
The moderate-to-severe AS diagnosis, while not officially recognized in the ASE guidelines, is commonly used. Last year at TCT, Genereux et al. published that this group represents about 30% of the SAS population – said otherwise, for every 100 SAS patients out there, we have another 30 with a “Moderate-to-Severe” (M-S) echo diagnosis from the reading cardiologist. This study also highlighted that moderate-to-severe patients are referred to heart teams at half the rate of severe AS patients but just as likely to diex. As recognition of the serious implications of aortic stenosis expands, there may be additional heart team referrals for the 80%+ of moderate-to-severe patients with symptomsxi. This is a tailwind that we expect to apply at half the rate to severe AS patients, accruing another 2-3% in heart team evaluations and 1-2% in AVRs for patients who meet “severe” criteria upon re-echo.Can We Mobilize This Information into Practice in Less Than 17 Years?
Studies showxii it takes 17 years for new guidelines to become common clinical practice. We will be in an exciting time for the treatment of AS if the guidelines change to recommend heart team evaluation and a shared decision-making treatment discussion for all severe AS patients, regardless of symptoms. At egnite, we can currently see that many severe and moderate-to-severe AS patients are in a medical management holding pattern because they are not convincingly severe and symptomatic enough to be scheduled for a heart team evaluation. If the symptomatic requirement falls away and clinical practice adapts across America, we estimate heart team clinics will see a 19-25% increase in heart team encounters and 5-17% increase in AVRs for severe AS on an ongoing basis.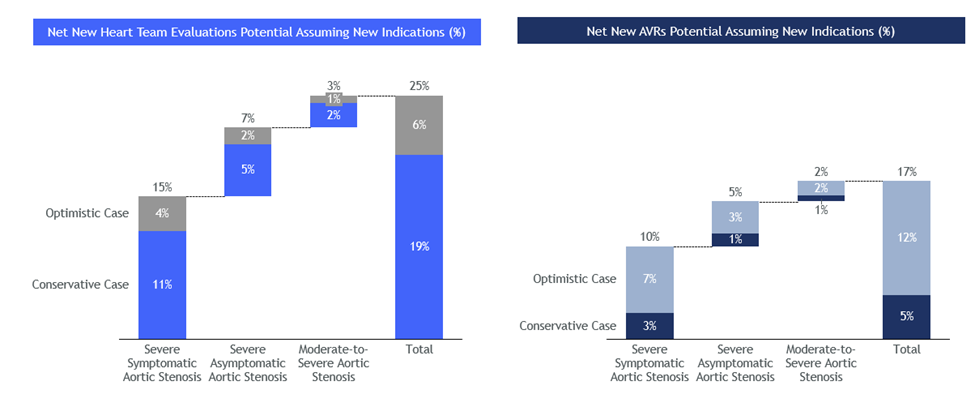
Final Thoughts
Health systems that can easily identify these medically managed asymptomatic and symptomatic AS patients will be best positioned to evolve access to care and beat the 17-year timeline. egnite’s expert CardioCare team helps health systems across the country benchmark their performance and mobilize to get with the AHA/ACC guidelines – if you’d like to talk, please reach out to me at jessica.neufeld@egnitehealth.com or check out our demo here and our team will get in touch with you. If you’d prefer a physician-to-physician discussion, we can connect you with a Medical Advisory Board member who would be happy to share their experience with CardioCare.
Congratulations to all the clinicians, scientists, engineers, trial managers, and innovators who helped bring this exciting data to the medical community. Most of all, thank you to the patients who participated in the research that brought this evidence to light.
Jessica Neufeld is the Chief Commercial Officer of egnite, Inc., a leading Cardiovascular Digital Healthcare company partnered with over 55 heart programs and 400 affiliated healthcare facilities nationally.
References:
i. Leon, MB, Smith, CR, Mack, M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597-1607
ii. Genereux et al. Acute Valve Syndrome in Aortic Stenosis. Structural Heart Journal October 2024.
iii. Internal egnite analysis performed October 2024.
iv. egnite’s Structural Heart Benchmarking Report, 2023.
v. egnite uses a sophisticated approach to determine if a patient is potentially a heart team evaluation candidate and potentially ‘treatable’ – in this group we exclude patients who are lost to follow-up, have had 2+ palliative care encounters, are manually dismissed for QOL/patient refusal/relocation or other reasons upon clinical chart review, have been treated with TAVR/SAVR/transplant, or expired. Kaplan-Meier curve analyses are applied to time-based statements such as ‘treated by 180 days’. Aortic stenosis severity is extracted from structured echo reports via egnite’s proprietary natural language process algorithms with over 99% accuracy.
vi. Why deem a patient with 1 symptom as ‘Unknown Symptoms’ status? egnite’s Medical Advisory Board consensus was that patients with 2 or more recent symptoms we can confidently label ‘Symptomatic’. Only one recent symptom can create debate amongst physicians at the average cardiology practice in America.
vii. Internal egnite analysis performed October 2024.
viii. Genereux et al. Acute Valve Syndrome in Aortic Stenosis. Structural Heart Journal October 2024.
ix. As an aside, we at egnite term these patients as ‘Unknown Symptoms’ given the literature that suggests that 33-66% of these patients with only 1 or 0 symptoms logged would prove to be symptomatic if exercise stress tested. Notably we see in our data that stress tests to elicit symptoms for SAS patients are rarely performed. Rafique et al. Meta Analysis of Prognostic Value of Stress Testing in Patients With Asymptomatic Severe Aortic Stenosis. AM J Cardiology 2009; 104:972-977.
x. Genereux et al. Mortality Burden of Untreated Aortic Stenosis. JACC October 2023.
xi. Internal egnite analysis performed October 2024.
xii. Westfall JM, Mold J, Fagnan L. Practice-based research–“Blue Highways” on the NIH roadmap. JAMA. 2007 Jan 24;297(4):403-6. doi: 10.1001/jama.297.4.403. PMID: 17244837.