BACKGROUND
Aortic valve replacement (AVR) is indicated in patients with severe aortic regurgitation (AR). However, certain clinical predictors may identify patients with less-than-severe AR at high mortality risk if untreated.
METHODS
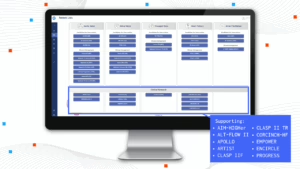
We analyzed patients >18 years of age with documented AR assessment in a deidentified real-world dataset from 27 US institutions with appropriate permissions (egnite Database; egnite, Inc). Diagnosed AR severity was extracted using a natural language processing-based algorithm. Cox multivariable analysis modeled the impact of key factors on untreated mortality according to AR severity.
RESULTS
81,378 patients were included for analysis. Hazard ratios (95% CI) for mortality were 1.26 (1.18-1.35) and 2.37 (1.96-2.87) for moderate and severe AR, respectively. Other significant predictors included left ventricular (LV) ejection fraction ≤55% (1.09 [1.02-1.15]), LV dilation (1.34 [1.21-1.48]), left atrial (LA) dilation (1.09 [1.03-1.16]), atrial fibrillation (1.11 [1.04-1.17]) and high B-type natriuretic peptide/N-terminal pro-B-type natriuretic peptide (1.71 [1.60-1.84]). Modeled mortality risk increased with the presence of these key predictors, either alone or in combination.
CONCLUSIONS
In patients with untreated AR, LV and LA remodeling and other cardiac damage predict mortality, both for severe and moderate AR. Further study is needed to determine whether AVR might be warranted in patients with less-than-severe AR with at-risk factors.
Généreux P, et al. Moderated abstract presentation at: American College of Cardiology 73rd Annual Scientific Session & Expo (ACC.24); April 6-8, 2024; Atlanta, GA.