“This is one of the first artificial intelligence-driven studies providing critical insights into care patterns for patients with moderate or greater AR in the community. The urgency for digital technologies to identify AR patients earlier and novel therapies to improve outcomes for this vulnerable patient population has never been greater.”
Assistant Professor at the Medical University of South Carolina and lead author of the study.
BACKGROUND
- Guidelines for management of aortic regurgitation (AR) suggest grading severity of disease using echocardiographic criteria 1,2
- Contemporary data on evaluation rates, aortic valve replacement (AVR) rates, and untreated mortality for patients stratified by degree of AR severity are lacking
- Prior literature to date has primarily focused on outcomes and/or treatment rates in
moderate to severe and/or severe AR 2,3
- Prior literature to date has primarily focused on outcomes and/or treatment rates in
METHODS
- De-identified real-world dataset (Jan 2018-Mar 2023) of 1,002,853 patients >18 years of age from 25 US institutions participating in the egnite Database (egnite, Inc., Aliso Viejo, CA, USA) with appropriate permissions
- Outcomes: 2-year rates of evaluation by the Heart Team, rates of treatment with AVR, and mortality without AVR were assessed using Kaplan Meier estimates (results compared via log rank test)
- Physicians were prespecified at the site level as members of the Heart Team
RESULTS
- Of the 1,002,853 patients, 845,113 had documented AR severity and were included in the main study analyses
- Median (interquartile range) time from index to death or censor was 405 (112-808) days
- Rates of evaluation by the Heart Team (95% confidence interval [CI]) at 2 years appeared low for patients with moderate-to-severe or severe AR
- 65.4% (63.3%-67.4%) for patients diagnosed with severe AR
- 43.5% (41.7%-45.3%) for patients diagnosed with moderate-to-severe AR
- Rates of AVR (95% CI) at 2 years also were low for patients with moderate-to-severe or severe AR
- 46.5% (44.2%-48.8%) for patients diagnosed with severe AR
- 19.4% (17.6%-21.1%) for patients diagnosed with moderate-to-severe AR
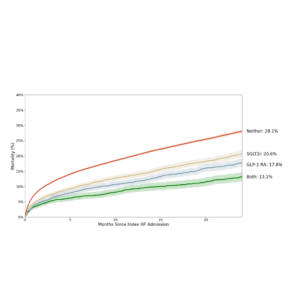
- Mortality for patients not treated with AVR increased with greater AR severity
- At 2 years, mortality (95% CI) was 20.7% (18.4%-23.0%) for patients with severe AR
- Two-year mortality (95% CI) for untreated patients with a left ventricular end systolic dimension index (LVESDi) ≤25 mm/m2:
- 17.1% (16.2%-18.19%) in moderate AR
- 22.9% (19.3%-26.3%) for severe AR
- For those with an LVESDi >25 mm/m2:
- 34.3% (29.2%-39.1%) in moderate AR
- 37.2% (24.9%-47.5%) in severe AR
CONCLUSIONS
- Untreated patients with at least moderate AR may have poor clinical outcomes
- Left ventricular dilatation (LVESDi >25 mm/m2) appears associated with substantial mortality, even with AR graded as “moderate”
- These data suggest that earlier referral and assessment by the Heart Team could be beneficial
- Despite the presence of clinically significant AR, patients are infrequently referred to the Heart Team
- Further studies are needed to determine the timing of intervention and the most optimal management of these patients
References
1. Otto CM, et al. JACC . 2021;77:e25 e197.
2. Nishimura RA, et al. Circulation. 2014;129:e521 e643.
3. Thourani VT, et al. Structural Heart. 2021;5:608 618
Amoroso NS, Sharma RP, Généreux P, Pinto DS, Dobbles M, Thourani VH, Gillam LD. Clinical journey for patients with aortic regurgitation: A retrospective observational study from a multicenter database. Presented at: TVT 2023: The Structural Heart Summit; June 7-10, 2023; Phoenix, AZ.