“These findings are extremely important and complementary to the recently presented EARLY TAVR Trial, published in the NEJM. The absence of symptoms was traditionally considered a sign of relative safety. However, this study shows how frequent acute valve syndrome is in patients undergoing AVR, and how patients would benefit greatly from intervention before symptoms appear.”
AIM
To describe the impact of clinical presentation among patients with aortic stenosis (AS) undergoing aortic valve replacement (AVR).
METHODS & RESULTS
We analyzed a real-world dataset including patients from 29 US hospitals (egnite Database, egnite). Patients >18 years old with moderate or greater AS undergoing AVR were included. Patients were classified in 3 groups according to the acuity and severity of clinical presentation prior to AVR: (i) asymptomatic, (ii) progressive signs and symptoms (progressive valve syndrome [PVS]), and (iii) acute or advanced signs and symptoms (acute valve syndrome [AVS]). Mortality and heart failure hospitalization after AVR were examined with Kaplan–Meier estimates, with results compared using the log-rank test.
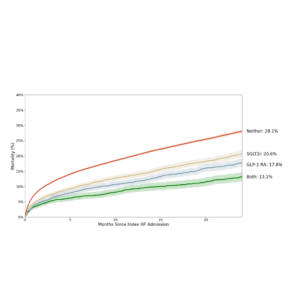
Among 2,009,607 patients in our database, 17,838 underwent AVR (78.6% transcatheter AVR, 21.4% surgical AVR). Age was 76.5±9.7 years, and 40.2% were female. Prior to AVR, 2504 (14.0%) were asymptomatic, 6116 (34.3%) presented with PVS, and 9218 (51.7%) presented with AVS. At two years, the estimated rate of mortality for asymptomatic, PVS, and AVS were 5.8% (4.6%-7.0%), 7.6% (6.7%-8.4%), 17.5% (16.5%-18.5%), respectively, and the estimated rate of hospitalization with heart failure for asymptomatic, PVS, and AVS were 11.1% (9.5%-12.6%), 19.0% (17.8%-20.2%), 41.5% (40.2%-42.8%). After adjustment, patients presenting with AVS had increased risk of mortality after AVR (hazard ratio, 2.2; 95% CI, 1.8-2.6).
CONCLUSIONS
From a large, real-world database of patients undergoing AVR for AS, most patients presented with AVS, which was associated with an increased risk of mortality and heart failure hospitalization.