BACKGROUND
Heart failure with a preserved ejection fraction (HFpEF) is characterized by frequent hospitalizations, and substantial mortality. While historically lacking effective therapies, newer treatments, including SGLT2 inhibitors (SGLT2i) and GLP-1 receptor agonists (GLP-1 RA), have shown potential benefits. However, the clinical course of HFpEF under these therapies remains incompletely characterized, warranting further investigation.
OBJECTIVES
To characterize the clinical course of HFpEF patients following heart failure (HF) hospitalization stratified by prescribed medical therapy class. Additionally, we examined trends in prescribing patterns since 2018.
METHODS
This study analyzes real-world data from U.S. health systems (egnite Database) under secondary research rights. Exemption from Institutional Review Board review was obtained for this study from the WIRB-Copernicus Group. Patients aged ≥18 years with an HFpEF diagnosis and a subsequent HF admission were included. Post-admission mortality was assessed using Kaplan–Meier estimates. Patients were stratified by SGLT2i and GLP-1 RA prescriptions at index hospitalization, with a time-varying Kaplan–Meier approach accounting for treatment changes if additional prescriptions were initiated post-index. Trends in prescribing patterns were assessed by tracking the proportion of HFpEF patients prescribed GLP-1 RA and/or SGLT2i at the time of HF admission from 2018 to 2024.
RESULTS
Among 11,362,626 patients in our database, 122,008 met the inclusion criteria (mean age: 75.0 ± 12.3 years, 59.3% female).
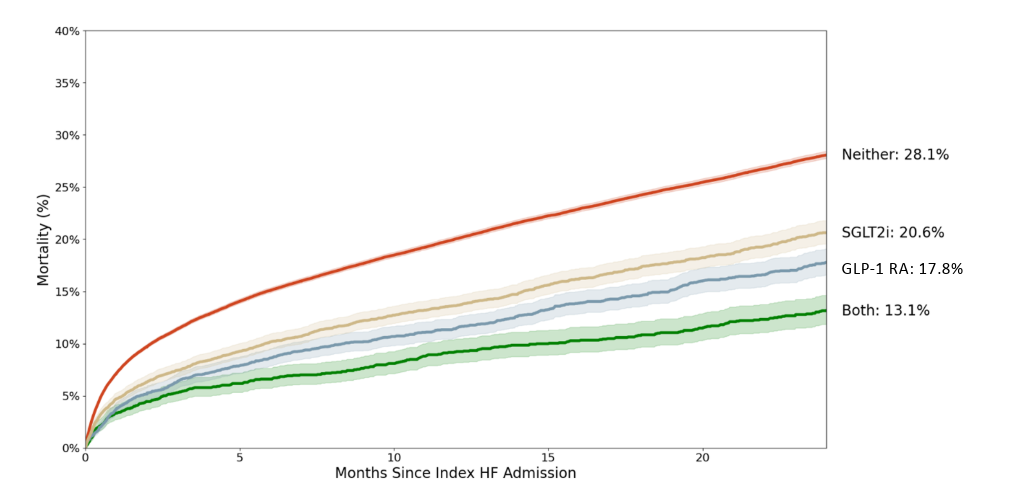
Estimated two-year mortality rates with 95% confidence intervals were as follows (Figure 1):
- 13.1% (11.8%-14.6%) for patients prescribed both GLP-1 RA and SGLT2i
- 17.8% (16.6%-19.1%) for GLP-1 RA only
- 20.6% (19.5%-21.8%) for SGLT2i only
- 28.1% (27.7%-28.4%) for neither
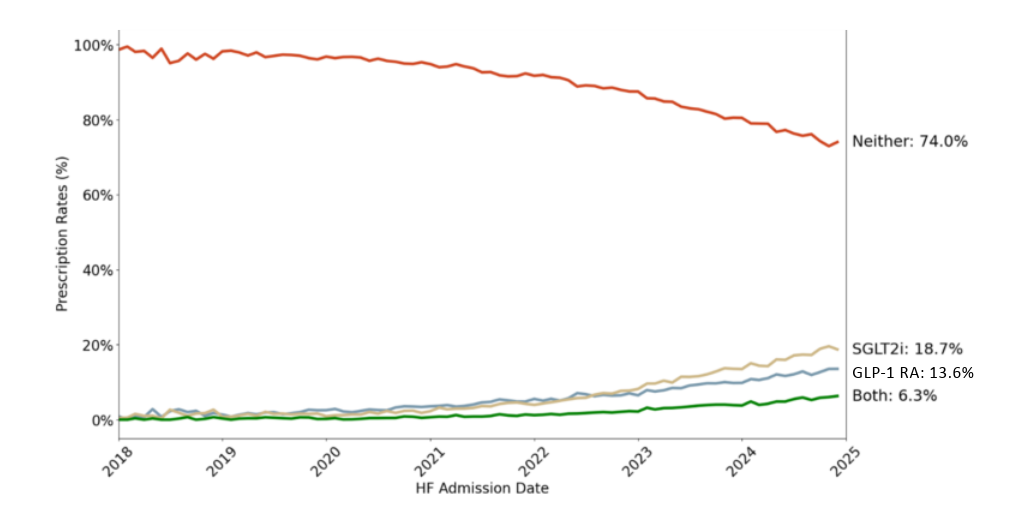
Prescription rates at the time of HF admission evolved as follows (Figure 2):
- January 2018: GLP-1 RA 0.9%, SGLT2i 0.5%, both 0.0%, neither 98.6%
- December 2024: GLP-1 RA 13.6%, SGLT2i 18.7%, both 6.3%, neither 74.0%.
CONCLUSIONS
In this large real-world HFpEF cohort, prescription rates for SGLT2i and GLP-1 RA have increased significantly since 2018. However, the majority of patients remained untreated at HF hospitalization. The absence of these prescriptions was associated with the highest two-year mortality rates, highlighting a critical gap in HFpEF management.



