“Over the last five years, new therapies to treat heart failure emerged with promising improvements in survival benefit. This study represents the first time we’ve seen an assessment of ‘5-class’ guideline-directed therapy — up to 4 foundational medication classes plus ICD/CRT-D therapy — for these patients. The next big challenge to overcome is implementing care at a time of growing disease burden and fewer clinical resources. Artificial intelligence powered insights, like those provided by egnite, will enable us to ensure appropriate care is provided to our entire patient population.”
John Mignone, MD, Ph.D.
Robert M. and Patricia Arnold Endowed Medical Director for Heart Failure and Co-Executive Medical Director Swedish Heart and Vascular Institute and lead author of the study.
BACKGROUND
Limited real-world evidence exists for outcomes with contemporary guideline-directed medical therapy (GDMT) or GDMT with implantable cardioverter-defibrillator (ICD)/cardiac resynchronization therapy defibrillator (CRT-D) therapy for patients with heart failure with reduced ejection fraction (HFrEF) and left ventricular ejection fraction (LVEF) ≤35%.
OBJECTIVE
The present study aimed to assess survival associated with GDMT or GDMT with ICD/CRT-D therapy.
METHODS
This retrospective observational study included real-world de-identified data from January 1, 2016, to December 19, 2023, from 24 U.S. institutions per participating institutional agreements (egnite Database; egnite, Inc., Aliso Viejo, CA, USA). Patients with a diagnosis of HFrEF and an echocardiographic study documenting LVEF ≤35% were included for analysis.
RESULTS
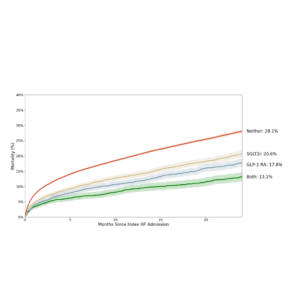
Of 43,591 patients with eligible index event of LVEF ≤35%, prescription history through ≥1 year preindex, and no ICD/CRT-D therapy preindex, mean ± standard deviation age at index was 71.2 ± 13.2 years; 14,805 (34.0%) patients were female. At 24 months, an estimated 99.1% (95% confidence interval [CI] 99.0%–99.2%), 89.9% (95% CI 89.7%–90.1%), 54.8% (95% CI 54.4%–55.2%), and 17.2% (95% CI 16.9%–17.5%), had ≥1, 2, 3, or all 4 GDMT classes prescribed, respectively; an estimated 15.7% (95% CI 15.3%–16.1%) had device placement. Of those without a device, by 24 months, an estimated 45.1% (95% CI 44.4%– 45.7%) had a documented LVEF >35%. Counts of GDMT classes prescribed as well as ICD/CRT-D device therapy were associated with lower mortality risk in this population, even after adjustment for patient age, sex, and comorbidities.
CONCLUSIONS
Both GDMT classes prescribed and device therapy were independently associated with lower mortality risk, even in the presence of more GDMT options for this more contemporary population.
Mignone JL, Alexander KM, Dobbles M, Fonarow GC, Ellenbogen KA. Outcomes with guideline-directed medical therapy and cardiac implantable electronic device therapies for patients with heart failure with reduced ejection fraction. Heart Rhythm. 2023;20(5):S138. doi: 10.1016/j.hrthm.2023.03.483